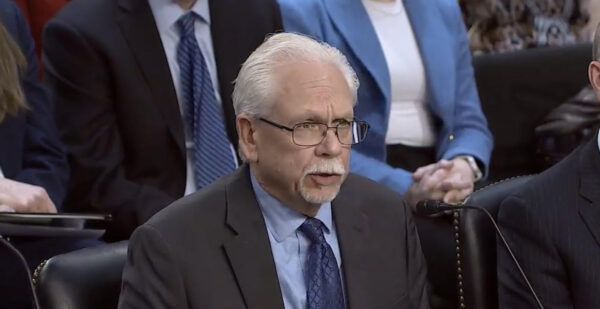
Editor’s Note: Piedmont HealthCare CEO Jeff Smith presented the following testimony before the U.S. Senate Special Committee on Aging on Wednesday, February 11, during a hearing exploring the causes of physicians giving up their medical practice.
BY JEFF SMITH
Chairman Scott, Ranking Member Gillibrand and members of the Committee:
Thank you for the opportunity to testify on how administrative and regulatory red tape fuels physician burnout and undermines patient access to care.
I am honored to speak on behalf of the Medical Group Management Association, MGMA, as its incoming board chair. MGMA has over 70,000 members across the United States, representing 15,000 medical group practices and more than 350,000 physicians. I am also CEO of Piedmont HealthCare PA, a physician-owned and led multi-specialty medical group bases in Statesville, N.C., with over 230 physicians and providers and almost 1,200 employees.
I have over 40 years of healthcare experience and I feel deeply passionate about this issue in part because I have seen its impact firsthand while working alongside my daughter, who now serves as a primary care physician in my practice.
MGMA has long advocated for reducing administrative burden and routinely surveys our members on administrative hurdles they face. Their feedback makes clear the connection between regulatory burden, a broken payment system and physician burnout.
In our 2026 survey, with over 230 respondent physician practices, more than half of practices report losing a physician to burnout in the past three years, and among those, over 75 percent say regulatory burden played a substantial role. This impacts patient access to care as it leads to longer waiting times, shorter visits, and practices becoming unable to accept new patients.
In my own practice I have increasingly witnessed more physicians being driven toward early retirement. Burden related to regulations impacts work-life balance as well, something I’ve seen with my own daughter, who often must complete these tasks at home after her children fall asleep.
While MGMA supports efforts to strengthen and expand physician training programs, addressing administrative and regulatory policies that are leading to physician burnout is critical to stem the tide on the front end and support physicians already in practice.
I would like to highlight the following burdens that I and other MGMA members are facing that significantly contribute to physician burnout:
♦ Medicare Advantage: Medicare Advantage has allowed beneficiaries to access new benefits and serve as an opportunity for innovation. However, as Medicare Advantage enrollment has increased, it has created daunting new challenges for many practices. MGMA members report audits, denials, prior authorization, and downcoding in Medicare Advantage as some of their top burdens in 2026.
There is also a significant lack of standardization across Medicare Advantage plans. We have had to hire whole teams dedicated to value-based care just to interpret what “quality” means for each payer.
♦ Prior Authorization: For years, one of the top cited regulatory burdens for medical groups has been prior authorization due to its impact on staffing demands, added costs, and impact on patient care. I oversee 75 offices in Charlotte metro area, and each practice has at least one staff members focused solely on prior authorizations.
MGMA members rank Medicare Advantage as the most burdensome payer. I appreciate the Chairman, Ranking Member, and many members of the committee for co-sponsoring the Improving Seniors’ Timely Access to Care Act. It is important to pass this widely supported legislation that would streamline prior authorization for Medicare Advantage.
♦ Additional Opportunities for Administrative Simplification: There are numerous additional opportunities to reduce duplicative and unnecessary regulatory hurdles. Reforming the Merit-based Incentive Payment System, or MIPS, in Medicare would be welcomed as complying with these requirements is a time-consuming and laborious process. Further, provider enrollment and credentialing in Medicare could be streamlined to better capture this data and lower practice costs.
♦ Medicare Payment: All of this regulatory red tape is exacerbated by the continued under-reimbursement of Medicare Part B. Financial stressors were the second largest contributing factor to physician burnout in our 2026 survey.
Given Medicare reimbursement’s frequent reductions due to outdated budget neutrality requirements and lack of an inflationary update, it is vital to pass legislation to comprehensively address these concerns.
♦ Increased Consolidation: The challenges discussed throughout this testimony coalesce to undermine the ability of independent medical groups to continue to operate and potentially lead many physicians to sell their practices.
One MGMA member relayed selling their practice to a hospital after 100 years of being physician-owned. Enacting long-term reforms would help lead to a more robust practice environment.
Conclusion
I sincerely appreciate the opportunity to testify today and share both my personal experience and other MGMA members’ experiences on how regulatory burden contributes to physician burnout. I look forward to answering your questions.



