BY DEBBIE PAGE
debbiepage.iredellfreenews@gmail.com
Mooresville physician James Allen III, in a Zoom meeting sponsored by Lake Norman Regional Medical Center, shared information to help businesses safely reopen as restrictions are lifted during the COVID-19 pandemic.
Allen, a local resident for 40-plus years, said “it was so nice to be in a position where I give back to you guys a little bit and try to guide y’all and your businesses and your employees through this mess and try to give you guys some guidance.”
Katie Yarborough, Corporate Health Program Manager for Davis Regional Medical Center and Lake Norman Regional Medical Center, introduced Allen, a Lake Norman Medical Group – Gateway doctor with 20 years of medical practice experience who also serves as medical director of LNRMC’s occupational medicine program.
Though no one set of guidelines will fit all business situations, Allen discussed the broad topics that will apply to most. He encouraged businesses to use him, LNRMC, and Davis Regional Medical Center as resources through the reopening periods.
“I really think it’s critical that we have a great relationship between our medical community and business leaders.”
COVID-19 IN PERSPECTIVE
Allen, acknowledging the horrible toll the COVID-19 virus has taken on the world, said, “We have to put this in perspective.” In a good flu year, Allen said 60,000 people die. In a bad year, such as in 2018, 80,000 died.
With the U.S. having surpassed 100,000 deaths attributed to COVID-19, Allen said that the country will experience more coronavirus-related deaths, but he noted that models have the United States peaking at about 140,000 deaths.
“We’re at roughly two times the mortality of the flu,” he said.
In North Carolina, with nearly 800 deaths as of June 1, Allen said “it’s really critical to understand that about two-thirds of these are in congregate facilities such as prisons or nursing homes in confined populations. Only about one-third are in the general population.
“Every death is horrible, but again, most of what of what we are seeing, like the flu, in terms of mortality, is going to be confined to these populations.”
Allen also wants people to understand the age disparity. “In North Carolina, 85 percent of people who have died are over 65 years old, and almost all of them have co-morbidities that are very significant.”
“Only 3 percent of deaths in North Carolina have occurred in individuals under 50 years old, so we need to kind of remember that as we go through this and as you look at the population of your businesses.”
WORKPLACE PROTECTIONS
Since each business is unique, Allen recommended developing a new guide to implementing workplace controls, polices, and procedures to deal with this viral threat.
Developing a hierarchy of controls to mitigate hazards includes engineering and administrative controls as well as enforcing safe work practices and employees’ use of personal protective equipment (PPE) to protect themselves and customers.
Allen outlined some workforce protections that will not “break the bank,” including:
♦ Considering using existing employees and supplies to manufacture barriers on production lines.
♦ Staying at least 6 feet apart during conversations, in locker rooms, hallways or corridors, and when entering/exiting the building.
♦ Not sharing drinks or food with co-workers in the break room.
♦ Regularly cleaning and disinfecting tools, especially when employees change workstations or move to a new set of tools.
♦ Avoiding carpooling, if possible.
♦ Allowing employees to wear N95 masks, surgical masks, or cloth masks.
♦ Providing hand hygiene stations and encouraging employees to wash frequently throughout their shift.
♦ Providing up-to-date education and ongoing training.
Allen noted that recommendations will change as more data and information become available, so staying up-to-date with employee training is particularly important.
The jury is still out on UVC wands’ effectiveness at killing COVID-19, but they may be useful. Just because nucleic virus residue is present does not mean transmissible virus is present on the surface.
Allen recommends mechanical (hands-on) cleaning with a sanitizing agent as the best route to take.
Allen noted that Lake Norman Medical Group is offering “Train the Trainer” consultations for employers implementing employee screenings at their workplaces. A trained nurse will come out and train people at workplaces.
The session includes a medical overview of COVID-19 and its symptoms, a demonstration on how to properly use thermometers, discussion of personal protective safety and PPE use, confidentiality and HIPAA concerns, and exposure and self-monitoring education.
EMPLOYEE SCREENING
Even though the loss of taste and smell is a newly noted sign of COVID-19 symptoms, Allen said employers should focus on the “bread and butter” symptoms when evaluating employee or customer health — such as fever, cough, and general feelings of sickness. “This is how you guys are going to have to screen.”
The CDC recommends that employees showing any of these symptoms should not be at work, which will lead to more absenteeism, changes in patterns of commerce, interrupted supply and delivery, and more planning on the part of employers to deal with these issues.
Allen noted, however, that the CDC has released new data that indicate widespread, asymptomatic cases of COVID-19.
At the very least, employers need to screen for symptoms, according to Allen. Depending on the nature of the business and consideration of the number of employees, employers should screen for fever, if feasible, which Allen considers critical. “That is going to catch the majority of these folks that are infected.”
Scanning thermometers are in short supply right now, so Allen advised employers to get whatever they can find. Fever guidelines for sending home employees range from 100.5 to 101 F.
If the employees do have significant fever at this level, Allen said they should get tested to determine if the illness is COVID-19 since many illnesses will cause a fever response. Business owners do not want to keep an employee from working if the illness is a short-range, non-COVID one.
“Symptoms, masks if you can, and screening for temps are the triad of detection or mitigation at this point for businesses,” he said.
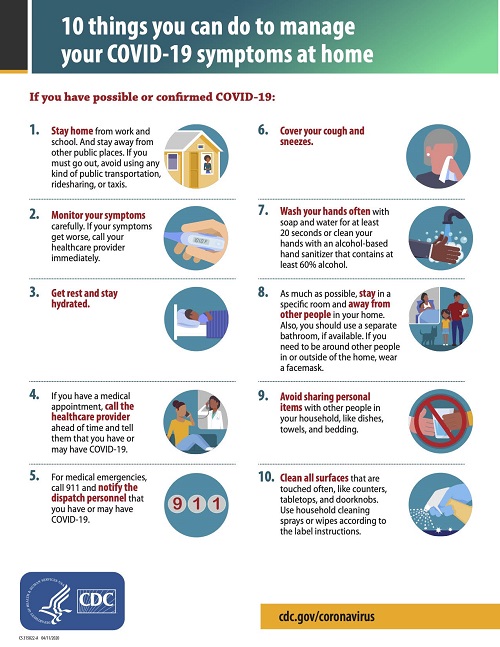
Another hurdle is following up with sick employees and determining when they can safely return to work. Allen provided a flyer employers can send home with suspected COVID-19 cases that details locations on where to receive care as well as tips for managing symptoms at home.
The employee should also use the NC Dept. of Health and Human Services Symptoms Log (https://epi.ncpublichealth.info/cd/lhds/manuals/cd/coronavirus/2_PUM_Symptom%20Self-monitoring%20Log.pdf?ver=1.2) to monitor and log symptoms. The employee will need to forward the form to the local Health Dept. once they are done with a 14-day home quarantine.
A sick employee can often be released to come back to work 14 days after initial diagnosis as long as they have seven consecutive symptom free days. Some employers may require two negative viral tests, 24 hours apart, but Allen said that policy would be expensive and perhaps not feasible because of testing availability.
EMPLOYEE TESTING
Employee testing also becomes an important issue. “In a perfect world, people would come to your business, you’d get a swab and know within 30 seconds if they were infected,” but Allen noted that level of ease of testing will not happen for a long time.
“Typically a patient will have symptoms. We’re not going to be able to catch everybody that’s asymptomatic or has atypical symptoms.”
Allen has COVID-19 patients who presented only with a headache and no other symptoms, but that is rare.
“The vast majority are going to be sick,” so screening and testing will need to be focused on those people.
Allen also noted that asymptomatic people will not spread the virus as readily since they are not coughing or sneezing.
Two kinds of tests are available for COVID-19: viral mRNA tests and antibody tests. A viral test indicated if the person has a current infection, while an antibody test indicates a previous infection.
However, an antibody test may not reveal a current infection because it can take one to three weeks after infection for the body to create antibodies.
“We do not know yet if having antibodies to the virus can protect someone from getting infected with the virus again or how long that protection might last.”
However, Allen believes that COVID-19, like other coronavirus strains that cause colds, will produce antibodies that will prevent reinfection, just like people develop immunity to a corona-type cold virus after getting it.
“This is not proven yet, but it should be exactly the same.”
He believes reports of reinfections are more likely persistent COVID-19 infections, not an actual reinfection, unless there is a compromised immune system that prevents normal creation of antibodies.
Unfortunately, the coronavirus strains that cause colds only create an immune response that lasts one to two years.
“We don’t know long these antibodies will last in people with COVID-19, whether it’s going to be a year or two, but it should be.”
Allen added that since testing is now relegated to the sick being triaged at hospitals and testing sites, first responders, and medical staff, testing all employees is going to be difficult. “There’s just not enough tests yet,” he said.
However, Allen predicted that soon people will have access to at-home tests, which will change the situation quickly.
Currently location testing centers and urgent cares are only offering COVID-19 tests to individuals with active symptoms, including significant fever and cough, and most are not offering antibody testing since their personal doctors can order and collect a blood sample for that test.
Testing services are available through:
Iredell Health System
557 Brookdale Drive, Statesville
Iredell Occupational Medicine
128 Plaza Drive, Mooresville
Kintegra Family Medicine (Formerly Statesville Family Medicine)
1022 Shelton Avenue, Statesville
Lake Norman Regional Medical Center
171 Fairview Road, Mooresville
Piedmont HealthCare Urgent Care – Mooresville
125 Days Inn Drive, Mooresville
Those desiring to take a COVID-19 test should call the facility before going there.
NAVIGATING FUTURE WITH COVID-19
Telemedicine, which Allen hopes will stay around, has been a valuable tool during the pandemic. New patient, sick visits, and follow-up visits are services offered for telemedicine, but annual or pre-employment physicals and workers’ compensation visits are not approved telemedicine visits.
Most insurance companies are covering telemedicine visits. However, patients should always call the insurance provider first to verify.
Hopefully, vaccines will soon be available, but Allen noted that coronaviruses are tricky. Though incredible strides on vaccines are being made by an army of researchers, Allen said, “I would be absolutely stunned as a scientist if we saw something before the end of the year.”
Therapeutics, including remdesivir by IV administration, are available, but no pills are yet available, though one company has isolated an antigen from the COVID-19 virus that might lead to a promising medicine.
Herd immunity, which involves allowing a large part of the population to develop COVID-19 antibody responses to prevent reinfection, could create a “barrier” to help tamp down the virus over time.
“It’s what we’re going to have to do. I think it’s so important to reopen businesses and let people out in our communities again, not without measure, not without being smart. If you are a compromised, at-risk person, you don’t need to be going to the mall.”
“We are going to have to let the population back out a little bit. We cannot hide in caves forever for a number of reasons, but the bear is still out there. It’s going to eat a few people — there’s no way around that.”
“But if we let enough folks out, less than 3 percent of mortality in North Carolina was in people less than 50, and that percentage had co-morbidities, whether it’s lupus, whether it’s cancer or something else.”
People less than 50 are not getting seriously hurt and will be okay, “so we have to contribute to herd immunity to get around this right now. And this is the time to do it – we need to do it in the summer time before the fall season comes.”
Mitigation measures are also effective to prevent COVID-19 infection. The CDC advises washing hands, maintaining a six-foot distance from others, and frequently cleaning and disinfecting surfaces.
The CDC also recommends use of non-medical, cloth-based face coverings in public settings where social distance cannot be maintained.
FOR MORE INFORMATION
As questions arise or for more information about securing a COVID-19 trainer, contact Yarborough at katie.yarborough@lnrmc.com or call her at (704) 660-4561.



